On this page, our nursing home lawyers will look at nursing home negligence lawsuits involving bedsores (also known as pressure sores or pressure ulcers). Bed sores are skin tissue wounds that develop when a person remains immobile in the same position for prolonged time periods. Bed sores can lead to infection and often death. Nursing home bed sore lawsuits are very common because bed sores are frequently the result of negligent care.
This post will explain how and why bed sores develop and examine the basics of how nursing home bedsore lawsuits work. We will also look at the average settlement value of these cases.
RELATED CONTENT:
Nursing Home Negligence Lawyers
Georgia Nursing Home Lawsuit
Chicago Nursing Home Lawsuits and Settlements
About Bed Sores
Bedsores, also known as pressure sores or pressure ulcers (decubitus ulcers) are tissue wounds that result from prolonged external pressure on certain points of the body. They are common when someone stays in the same position for a very long time with little movement. When this happens, the weight of the body puts external pressure on the skin and tissue, restricting blood and oxygen flow to the area. This eventually causes the tissue wound to develop.
Pressure sores can develop whenever the blood supply to the skin is cut off for more than a few hours. Elderly residents in nursing homes, assisted living facilities, or hospitals are particularly vulnerable to bed sores because residents are immobile and reliant on staff to move them regularly, and this very rarely happens as much as it should.
Depending on the severity of the bedsore, the person’s physical condition, and the presence of other diseases (such as diabetes), bedsores can take days, months, or even years to heal. They may need surgery to help the healing process.
There are certain pressure points on the body where bedsores typically develop:
- Buttocks (sacral)
- Heels of the feet
- Shoulder blades
- Back of the head
- Backs and sides of the knees
Bed Sore Stages
Bed sore wounds are classified into 4 recognized stages. Each stage generally corresponds to how deep the pressure wound goes into the tissue. The depth of the wound also generally corresponds to the severity of the pressure sore. The deeper the bed sore gets, the more serious it becomes.
Stage 1: The wound is at the surface. The skin appears red and warm to the touch (or purple in people with darker skin). The wound may ache or itch.
Stage 2: A Stage 2 bed sore will cause the skin to appear more damaged, often with open sores are the surface that look like scrapes or blisters. The skin around the outside of the wound area will become discolored and the wound will begin to cause very significant pain.
Stage 3: When the tissue damage begins to get deeper, the wound area will begin to sink and look like a crater as a result of the loss of subcutaneous tissue. Stage 3 bed sores are referred to as “full thickness” wounds.
Stage 4: A bed sore is classified as Stage 4 when the wound gets so deep that it extend to the muscles and bones. This is when systemic infection becomes a major risk factor.
Prevention and Treatment of Bedsores
Preventing bedsores from developing is very important, particularly for elderly nursing home residents. The key to avoiding bedsores in elderly residents who are immobile is to regularly move and reposition them to ensure blood circulation to the pressure points on the body. This requires a lot more than simply rotating the patient from a horizontal to a vertical position 2 times a day. Immobile residents need to be repositioned every few hours, and walked around if possible. Good nutrition and keeping the skin clean and moisturized is also important to prevention.
Once pressure sores develop, initial treatment calls for the immediate relief of pressure on the developing wound to prevent it from getting worse and begin healing. There are special types of hospital beds that can be used to alleviate pressure on certain areas of the body when a patient is laying down.
Protecting the wound with medicated dressings of gauze and keeping it clean are also standard treatment methods. If necessary, the wound may need debridement, the removal of dead, damaged or infected tissue, to avoid sepsis, necrotizing fasciitis, and gangrene. Surgery, too, may be necessary in severe cases.
Nursing Homes Have a Duty to Prevent and Treat Bedsores
Some bedsores are clinically unavoidable. However, a majority of bedsore cases in nursing homes are entirely avoidable and the bedsores are simply the result of negligent care. Nursing homes and other elder care facilities have an affirmative duty to prevent bedsores from developing. This requires checking for bedsores and regularly moving patients to ensure blood circulation.
Bedsore protocol also calls for immediate and appropriate intervention when signs of a developing pressure ulcer first appear. This typically involves the relief of external pressure on the wound, often with the use of a specialty bed. The obligation of a nursing home to prevent and treat bedsores is set forth very clearly in the federal regulations that set forth care standards for Medicare and Medicaid recipients. These regulations state that nursing homes are obligated to:
ensure that (1) a resident who enters the facility without pressure sores does not develop pressure sores unless the individual’s clinical condition demonstrates that they were unavoidable; and, (2) a resident having pressure sores receives necessary treatment and services to promote healing, prevent infection and prevent new sores from developing.
Proving a Bedsore Negligence Lawsuit
Bed sores frequently result in nursing home negligence lawsuits because if a resident develops a bed sore, the injury itself is often evidence of negligent care. To succeed in a nursing home bedsore lawsuit, the plaintiff must show that the nursing home was negligent in failing to prevent the bedsore from developing, and/or failing to properly treat the bedsore once in developed.
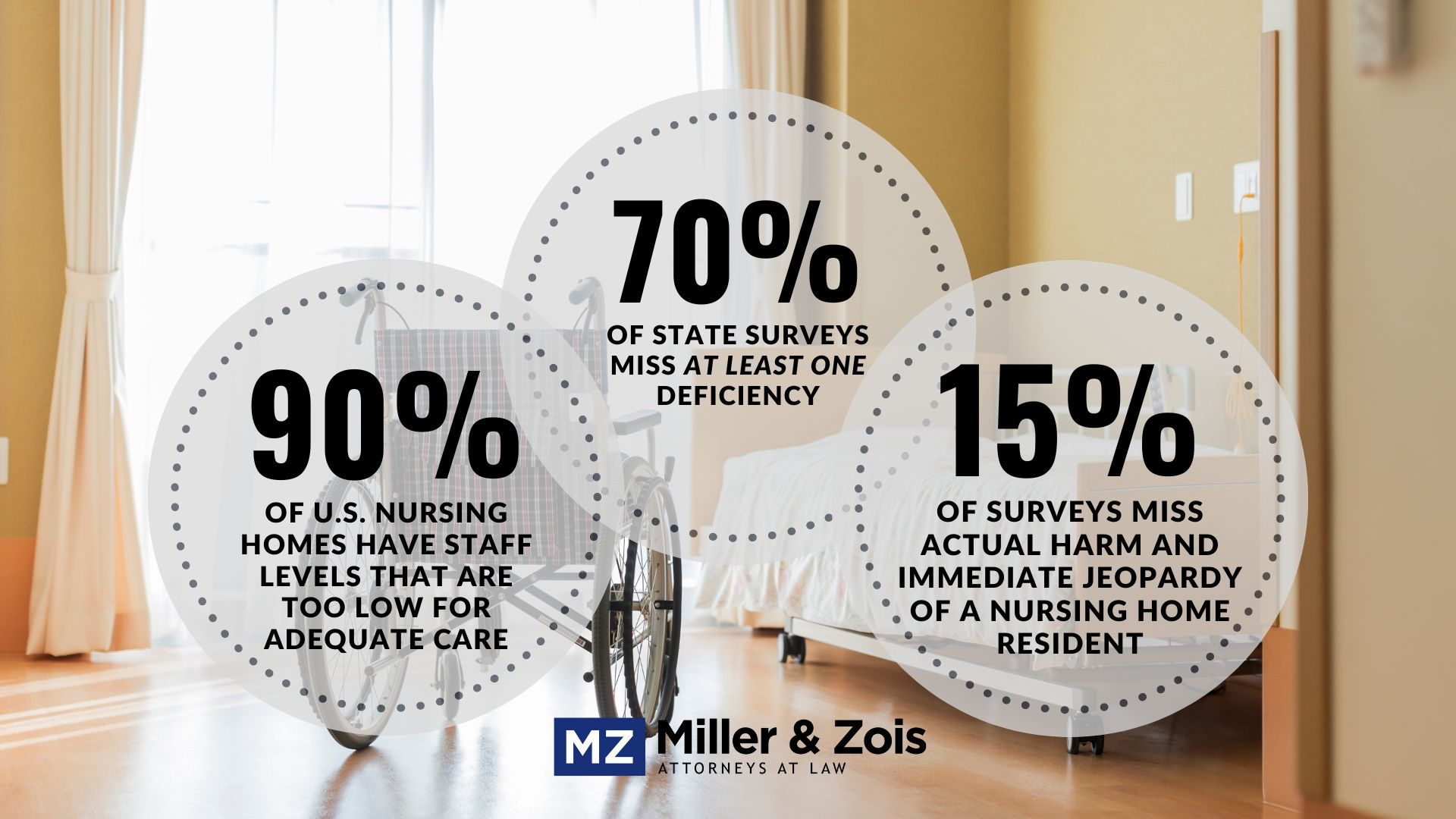
Most bedsore lawsuits allege that the nursing home was negligent in failing to prevent the pressure wound from developing by regularly moving immobile residents to ensure blood circulation. Exactly what constitutes “regularly moving” a resident will depend on the circumstances, but in most nursing home cases this is easy to establish because nursing homes are notorious for this type of patient neglect. Whether through understaffing or simple neglect, residents at nursing homes rarely get the level of care necessary to prevent bedsores.
Settlement Value of Nursing Home Bedsore Lawsuits
Around 17,000 bedsore negligence lawsuits are filed each year, making it one of the most frequently litigated injuries. Nursing home bedsore lawsuits have a very high rate of success compared to other types of medical malpractice cases. The plaintiff success rate in bedsore lawsuits against nursing homes is over 85%.
A very high percentage of nursing home bedsore cases are resolved in a settlement. Nursing homes rarely take bedsore cases to trial, mainly because nursing homes have such an abysmal reputation for neglect that they are very vulnerable defendants. The average settlement payout value for nursing home bedsore lawsuits is around $260,000.
Bedsore Settlements and Verdicts
Below are summaries of recent verdicts and publicly reported settlements from nursing home bedsore negligence cases form around the country.
$215,000 Settlement (Pennsylvania 2024): An elderly nursing home resident developed sacral pressure sores from which she eventually died of sepsis. The lawsuit alleged that the nursing home was chronically understaffed and that it routinely failed to reposition and turn the decedent in her bed so as to avoid the pressure sores from developing. The reason for the lower settlement value of this case is because of the decedent’s age.
$225,000 Settlement (Pennsylvania 2024): A 54-year-old male died due to complications related to pressure sores that developed on his right buttock while he was a resident of a skilled nursing facility owned and operated by defendants. The decedent’s estate claimed the defendants were negligent in failing to provide pressure sore prevention, failing to obey physician’s orders and failing to routinely reposition the plaintiff.
$9,000,000 Verdict (Maryland 2023): An elderly pastor was admitted to a nursing home after suffering a stroke that left him partially disabled. While at the nursing home he was severely neglected by the staff who often left him unattended and failed to move him on a regular basis. As a result of this neglect, the man developed a bed sore which eventually developed into a sepsis infection and caused his death. A jury in Baltimore County awarded $9 million, although that amount will be reduced by Maryland’s cap on non-economic damages.
$175,000 Settlement (Pennsylvania 2023): Elderly nursing home resident was admitted to the defendant facility with no skin ulcerations and was unable to communicate and confined to a bed. She later died from sepsis caused by bedsores that she developed while at the nursing home. The lawsuit alleged that the nursing home staff failed to routinely move the decedent to allow for proper circulation and to prevent skin ulcerations. The estate claimed defendant staff failed to perform routine skin checks, failed to provide the decedent with a low-pressure air mattress, failed to notify physicians that bedsores had formed and failed to timely consult with a wound care specialist.
$30,912,000 Verdict (California 2023): An 86-year-old man underwent surgery for a fractured hip and stayed at the defendant’s nursing facility afterwards during his recovery. During his two-week stay at the facility he developed two unstageable heel pressure sores, one of which was discovered to be a to-the-bone stage IV pressure sore. He died almost a year later and reportedly suffered with the sores, and resultant pain and debility, during the last year of his life. The lawsuit accused the nursing facility of negligent failing to prevent the pressure sores from developing by regularly moving him. This case is a good example of the extreme risk nursing homes take when they ask a jury to determine their fate.
$250,000 Settlement (Illinois 2023): An 89-year-old female nursing home resident died from an infection related to multiple pressure sores. The estate filed a lawsuit claiming that the defendant nursing home failed to properly assess the decedent’s risk for pressure sores and failed to provide proper wound care treatments as ordered. The case was quickly settled.
$650,000 Settlement (South Carolina 2021): Elder male developed a pressure sore while at the defendant hospital. He developed additional pressure sores which became necrotic after he was transferred to the defendant assisted care facility. The wounds developed into sepsis and he died. The lawsuit alleged that the hospital and nursing home were negligent in failing to reposition him every 2 hours and provide proper nutrition. The cases was eventually settled with each defendant contributing half.
$75,000 Verdict (Florida 2020): An elderly male resident at the defendant nursing home developed a pressure sore on his right heel that became gangrenous and caused a systemic infection. He sued the nursing home alleging that it was negligent in allowing the wound to develop and then progress. The nursing home claimed that the infection was caused by the man’s pre-existing vascular disease.
Hire a Nursing Home Lawyer
If you have a nursing home bedsore negligence case, contact our nursing home lawyers today. Contact us online, or call at 800-553-8082.
 Lawsuit Information Center
Lawsuit Information Center